Case:
A 55 year-old male with history of hypertension presented to the ER with a chief complaint of "not feeling well" with leg pain and paresthesias. Upon further questioning, the patient admitted to waking up that morning with diaphoresis and pain in his upper back that had now migrated to his chest and upper abdomen. His exam was significant for bradycardia and diminished pulses in all four extremities. He had no murmur, no abdominal tenderness and no neurologic deficits. A bedside echo and ultrasound of the aorta was obtained and showed the following:
Case conclusion:
The patient's ultrasound confirmed the diagnosis of an aortic dissection and an aneurysmal ascending aorta. Aggressive blood pressure control was initiated. A CT was obtained to further characterize the dissection and showed a Type B dissection with an origin at the level of the left subclavian artery, extended to the distal right external iliac, and had propagated into the celiac, superior mesenteric and right renal arteries. The patient was admitted to the CICU with cardiothoracic surgery on a nicardipoine drip and is scheduled aortic root replacement and CABG.
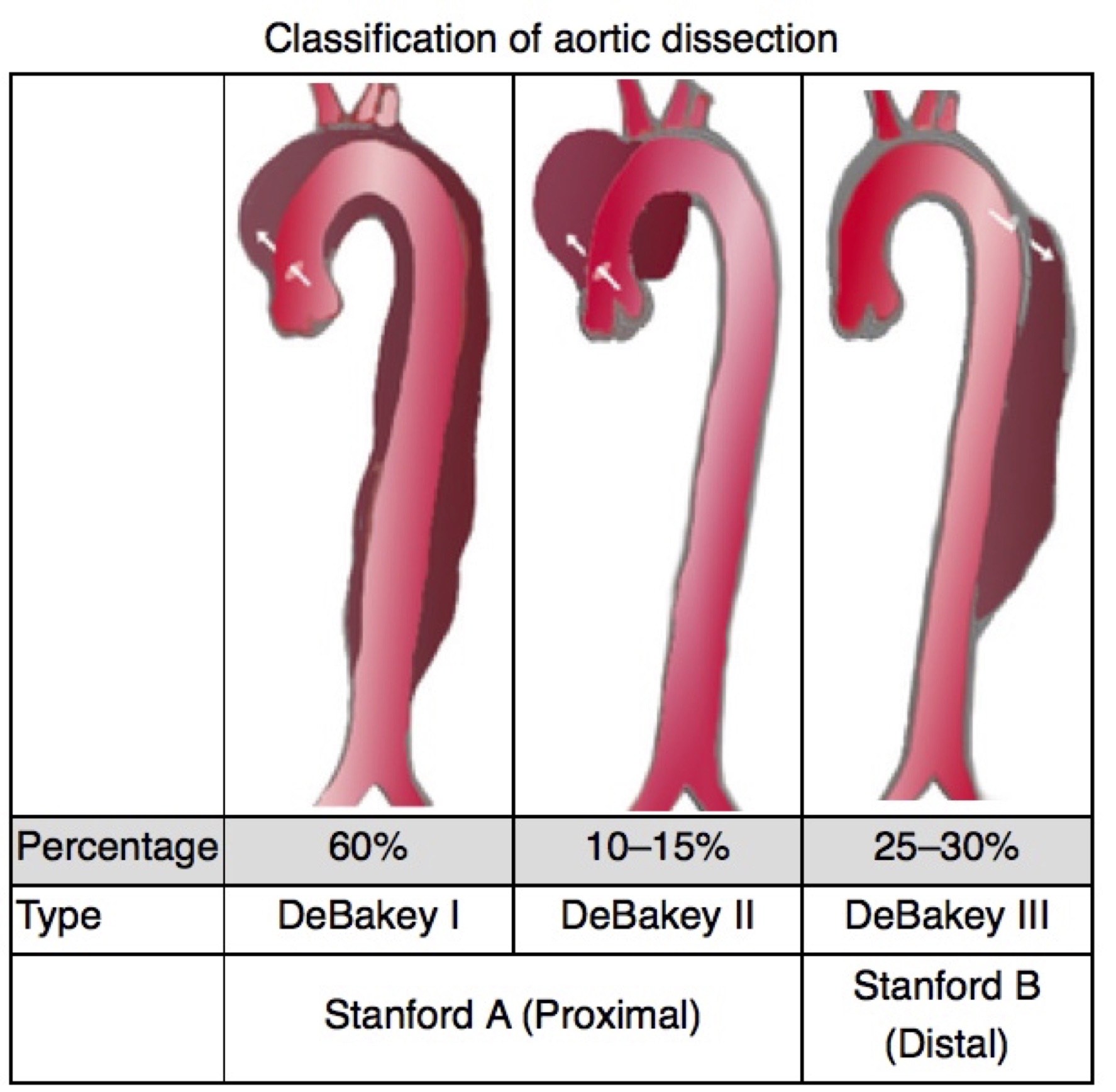
Classifying aortic dissection
Type A dissections originate in the ascending aorta and may either be confined to the ascending region of the aorta or extend into the descending aorta
Type B dissections do not involve the ascending aorta
Transthoracic Echo for Aortic Dissection
Parasternal long axis view (PSLA):
· Aortic outflow tract size: measure the widest visualized region of the aortic root, from inner wall to inner wall. An aortic outflow tract diameter of >3.5 cm is highly sensitive for an aneurysmal aorta and aortic dissection in both men and women.
· Presence of an intimal flap: while it can be challenging to identify, the finding of an intimal flap within the proximal aorta is pathognomonic for aortic dissection. A true flap will be seen to undulate within the aortic lumen and color flow can be used to demonstrate the presence of the false lumen. Beware of artifact mimicking a flap within the ascending aorta. Reverberation artifact from the aortic wall may appear as a line within the aortic root, but it will not have any fluttering or waving movements characteristic of a true dissection flap.
o Other tips to increase your detection rate of proximal aortic dissection flaps include examining the visualized region of the descending thoracic aorta on the PSLA view, which is seen deep to the left atrium.
o Also consider using the suprasternal notch view to obtain a coronal view of the aortic arch.
· Pericardial effusion: evaluate for the presence of a pericardia effusion and, if present, findings of tamponade. Check out the previous post to review ultrasound evaluation for tamponade at https://www.templeemergencyultrasound.com/weekly-case-challenge/2018/3/25/a-collapsing-heart.
Abdominal aorta:
· Transverse view: start in the epigastric region, as cephalad as possible, and provide firm pressure to evaluate the proximal abdominal aorta in a transverse orientation. In this region, watch carefully for the presence of an undulating luminal flap. Aortic dissection is generally a disease of the thoracic aorta, making the most proximal aspect of the aorta vital to examine.
· Sagittal view: rotate the probe 90 degrees in the epigastrium to visualize the long axis view of the aorta, again looking for an intraluminal flap. If bowel gas prevents visualization from the anterior aspect of the abdomen, the long axis of aorta can be obtained by looking from the midaxillary line, using the liver as an acoustic window.
Findings of any of the above abnormalities (widened aortic root, pericardial effusion, intimal flap in the aortic root or abdominal aorta), has a sensitivity of about 96% for aortic dissection and a specificity of 90.8% (Gibbons et al).
-Allison Zanaboni, M.D., Emergency Ultrasound Fellow
References:
Gibbons R, Smith D, Mulflur M, Dai T, Satz W, H. Goett, and T. Costantino. "364 Point-of-Care Ultrasound for the Detection of Aortic Dissections in the Emergency Department." Annals of Emergency Medicine 70.4 (2017)
Fojtik J, Constantino T, Dean A. The Diagnosis of Aortic Dissection by Emergency Medicine Ultrasound. J Emer Med 2007; 32: 191-96.
Kaban J, Raio C. Emergency Department Diagnosis of Aortic Dissection by Bedside Transabdominal Ultrasound. Academic Emerg Med 2009; 16: 809-10
Alter P, Herzum M, Maisch B. Echocardiographic Findings Mimicking Type A Aortic Dissection. Herz 2006; 31.2: 153-55.
Sobczyk D, Nycz K. Feasibility and Accuracy of Bedside Transthoracic Echocardiography in Diagnosis of Acute Proximal Aortic Dissection. Cardiovascular Ultrasound 2015; 31.