The Case
67yoF with history of CHF and COPD on 2L O2 at home presents with hypoxia and worsening shortness of breath with exertion. Patient reports she stopped taking her diuretic about one week ago and noting a productive cough over the past five days. She reports possible subjective fevers last night but denies recorded fever. Patient denied sick contacts, leg swelling, chest pain, and recent travel. In triage, patient had an O2sat of 84% on room air but improved to 96% on her home 2L NC of oxygen. Bedside ultrasound showed the below findings:
The Diagnosis
Lung ultrasound was significant for scattered B-Lines and a B-Zone in the right upper lung (RUL). There was also noted a pleural effusion in the left lower lung (LLL). The pleural lines were noted to be thickened and irregular. XR had increased interstitial markings but no changes in the bases. Patient had a CT showing ground-glass opacities. Patient was sent for COVID testing following admission and her test resulted POSITIVE.
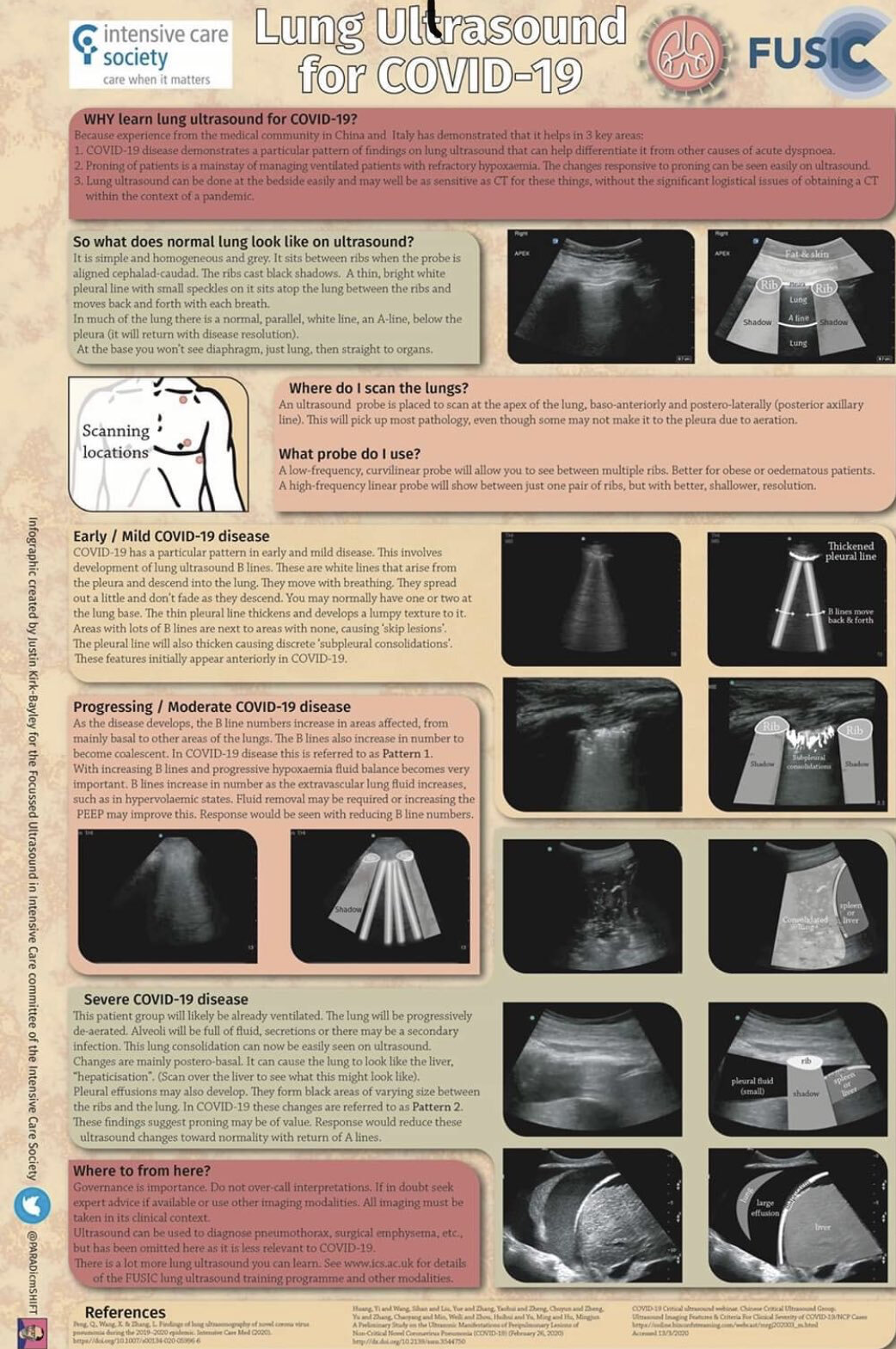
Basics of Lung Ultrasound
Our usual protocol is to set the depth to at least 12cm to adequately evaluate different areas of the lung. By using the curvilinear probe in sagittal views, it is possible to view multiple sections of the lung through the intercostal spaces between the ribs. Our typical 4 areas we check are right upper lung (RUL), left upper lung (LUL), right lower lung (RLL), and LLL (left lower lung). The upper lung zones are visualized mid-clavicular and the lower zones are evaluated mid-axillary. The linear probe can also be used for a higher resolution view of the pleural line.
Lung Ultrasound for COVID-19
Reports suggest Lung Ultrasound may have earlier findings than CXR with COVID infection. These same reports suggest more lung areas are required adequately evaluate for the changes seen with the COVID-19 disease process. Because of this, we recommend a scan to include 8-areas: right upper lung (RUL), right mid-lung (RML), right lower lung (RLL), right posterior lung (RPL), left upper lung (LUL), left mid-lung (LML), LLL (left lower lung), left posterior lung (LPL).
A quick view of the heart can evaluate for causes that may lead to pulmonary edema. In the absence of RV strain of the changes of CHF, positive findings in the lung are more concerning for a viral pneumonia. In patients with CHF, check the IVC as plethora (>2cm, no collapse) is more consistent with volume overload. Collapse and <1cm is more consistent with an infectious process. Lung ultrasound should always be done with cardiac and IVC ultrasound to help narrow the differential of undifferentiated dyspnea.
Mild Disease (Early Stage)
Early stages of the disease have been noted with the appearance of B-Lines. B-Lines are vertical hyperechoic lines that move with lung-sliding and extend to the bottom of the screen. They can be described as “search lights” or “laser beams”. The pleural line is usually smooth but with COVID will become thicker and more irregular (areas that appear jagged like a saw-tooth).
Moderate Disease (Progressing Stage)
As the disease progresses there is an increased number of B-Lines and may even coalesce into a B-Zone (thick area of B-Lines).
Severe Disease
Pleural effusions may develop, and the lung will develop areas of consolidation especially in the bases. Areas of consolidation may appear as hepatization of the lung (liver-like appearance). These changes occur most commonly in the inferior and posterior segments of the lung.