Case:
61 yo F with hx of COPD, pulmonary hypertension with only mild reduced RV function on recent echo, and recurrent DVT/PE with IVC filter in place, known to be non-compliant on Coumadin, presented with atraumatic left leg pain and swelling for one week, associated with worsening chest pain and shortness of breath. On exam, she was tachycardic, had O2 sat on RA around 90% and had left lower leg swelling to the level of the knee with tenderness to palpation of the thigh and in the popliteal fossa.
Given concern for recurrent VTE, a bedside echo and DVT study were performed.
Case conclusion:
The POCUS shows evidence of DVT in the left common femoral and popliteal veins, and the echo is significant for marked RV dilation with septal bowing and a D-sign. Despite the patient's history of PAH, her recent echo showed no evidence of severe RV dysfunction, raising the suspicion that the patient had acute right heart strain secondary to VTE. Based on these ultrasound findings, the PERT team was activated, the patient was admitted to medicine and lovenox was initiated.
The patient underwent CTA that showed multiple PEs, both acute and acute on chronic, and a subsequent lower extremity doppler confirmed acute on chronic LCF DVT with acute clot from the distal femoral vein and below.
Take aways:
EMBU for DVT:
As was mentioned in last week’s Case of the Week, the two-point compression study to evaluate for lower extremity DVT is a validated technique for use in the ED. Compress the CFV from above the level of the saphenous vein branch point distal to where the vein splits into the superficial and deep femoral veins, compressing every 1-2 cm. Compress the popliteal vein from the popliteal fossa distal until the vein divides into it’s 3 branches. The DVT study is negative in the views if the walls touch completely. If the vein is non-compressible, it is a positive study regardless if hyperechoic clot is visualized or not.
If the study is negative, the patient EITHER needs a NEGATIVE D-Dimer, OR needs to be counseled to have repeat imaging in 1 week to exclude propagation of a calf clot.
In this case, you can see that the associated arteries are being compressed, yet the veins do not collapse. Some echogenic material can be seen within the CFV, as well as at the periphery of the pop.
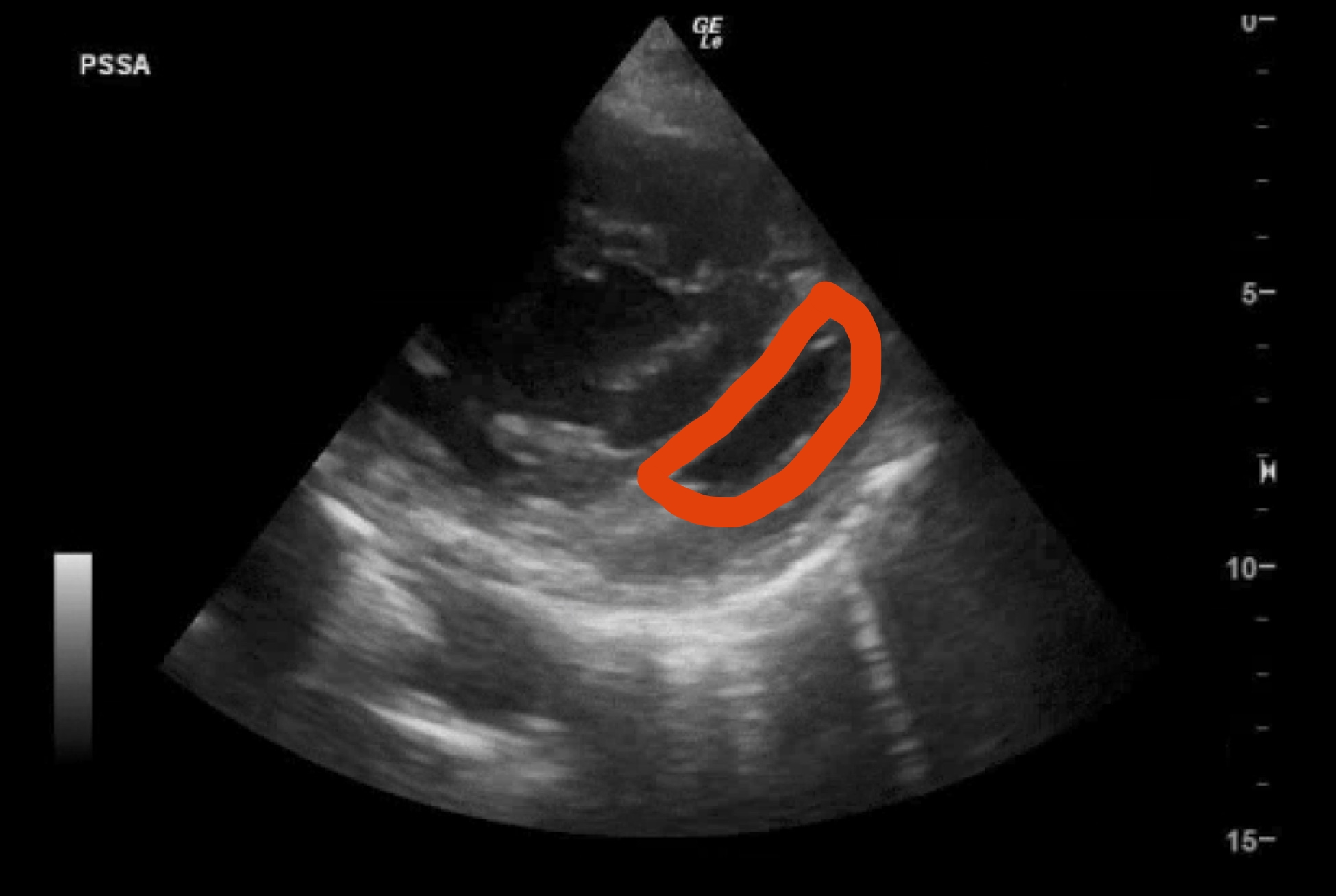
EMBU for right heart strain:
When using bedside echo to diagnose PE, you're looking for signs of right heart strain as indirect markers of PE. In patients who have history of RV dysfunction or chronic lung disease, the echo may show signs of RV dysfunction not related to PE, but in the appropriate clinical context, look for the following findings:
- RV dilation: a normal RV should be about 60% the size of the LV; if the RV is the same size or bigger than the LV, consider true RV stain
- D-sign: when RV pressure increases, it will deform the septum, pushing it into the LV. On PSSA, the LV will appear to look like a D rather than an O, as can be seen on the echo image above
- McConnell's sign: in the apical view, akinesis of the RV free wall can be seen, with normal apex contraction
- TAPSE: tricuspid annular plane systolic excursion. Measure in the apical 4 chamber view using M mode with the cursor over the junction of the tricuspid valve and either the RV free wall or septum. Measure the distance that this plane moves. Normal is >16mm
In this case, the large RV that dwarfs the size of the LV and flattens and then bows the septum into the LV cavity can be seen.
Final Pearls:
-Use 2 point compression US to evaluate for DVT in the ED
-When trying to diagnose PE, look for RV size greater than LV, D-sign, McConnell's sign, give TAPSE a try, and don't forget to look for DVT
-Allison Zanaboni, MD, Emergency Medicine Ultrasound Fellow