Case:
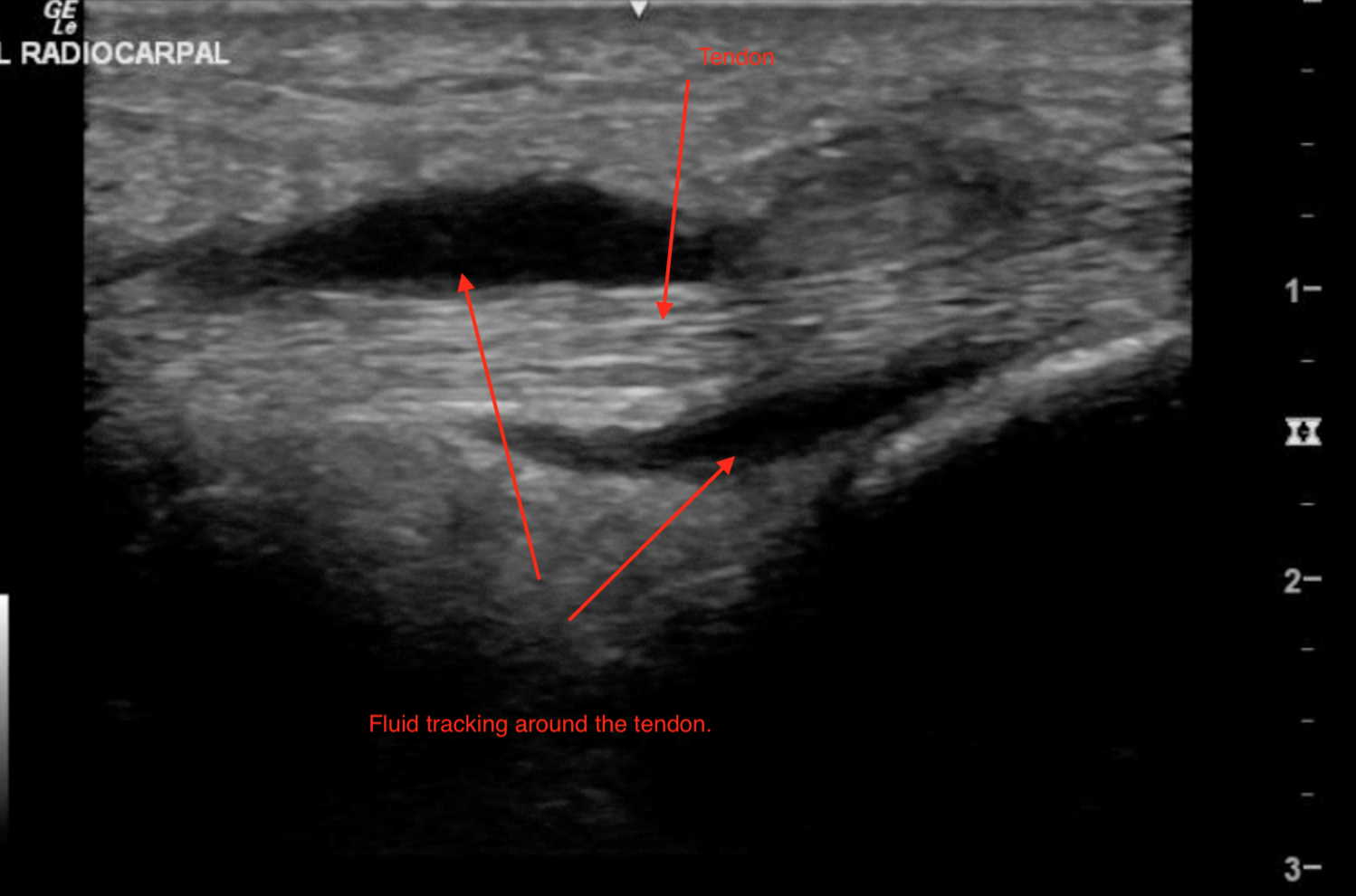
56-year-old male with history of poorly controlled diabetes presents to the emergency room after 3 days of increasing pain, swelling, warmth, and erythema to the dorsum of his wrist. He endorses pain with movement and touching of the wrist. He denies fevers, but has experienced chills and general malaise. Ultrasound at the bedside revealed the following images.
The anatomy of the wrist and associated pathology (below).
This case demonstrates the rare case of extensor tenosynovitis in a middle-aged male with poorly controlled diabetes mellitus. In this example, POCUS provided us the ability to thoroughly assess suspected underlying pathology and visualize the joint space, tendon, and surrounding tissues for inflammation and fluid. In our images the distorted anatomy of the extensor tendon is clearly visualized, as it is surrounded by abscess and tissue edema. Perhaps more importantly, we can visualize that the joint space itself is intact, ruling out septic arthritis as a possible diagnosis. In this example, a blind attempt at joint aspiration may have led to the seeding of the radialcarpal joint space by the abscess as the needle was advanced through the soft tissues.
Unfortunately, physical exam alone can be unreliable in cases of extensor tenosynovitis and the lesion can be mistaken for a simple cellulitis, as cases may lack some of the typical characteristics of flexor tenosynovitis. Be suspicious of diagnosing soft tissue infections of the extensor areas of the wrist or ankle without POCUS, as these are the most common areas of occurrence.
Case Conclusion:
Under ultrasound guidance, the abscess was directly visualized and decompressed using a simple needle aspiration technique. The patient experienced immediate pain relief and was promptly admitted to the hospital for antibiotics and orthopedic management.
References:
Newman ED, Harrington TM, Torretti D, Bush DC. Suppurative extensor tenosynovitis caused by Staphylococcus aureus. J Hand Surg Am 1989; 14:849.